

Polypharmacy and Its Burden on Aging Kidneys
Thirty-eight percent of Americans aged 65 or above have chronic kidney disease (CKD) according to the Centers for Disease Control and Prevention1. People with high blood pressure, heart disease, diabetes, obesity and a family history of kidney diseases are more prone to having kidney illnesses.
Why Is Kidney Disease Prevalent in the Elderly?
The kidneys are made up of millions of tiny filtering units called nephrons, which remove metabolic waste and excessive water from the blood. But as we age, the number of nephrons gradually decreases and that affects the rate at which blood is filtered.
Extended Reading: 10 Frequently Asked Questions About Kidney Health
Age-related changes aside, seniors are also more likely to have chronic health conditions that require the use of multiple medications. Statistics show that polypharmacy — taking five or more drugs concurrently — is observed in 44% of the elderly2. Polypharmacy not only increases the risk of drug interactions, but also burdens the aging kidney.
Impact of Polypharmacy on Kidney Function
To learn more about how polypharmacy affects the kidney health of seniors, we interviewed Dr. Wendy St. Peter, PharmD, a member of the National Kidney Foundation’s (NKF) Scientific Advisory Board, and Dr. Holly Mattix-Kramer, MD, president of NKF’s Board of Directors.
Dr. St. Peter: Polypharmacy is problematic because it increases the chance of drug-drug or drug-food interactions and additive side effects. Many drugs are removed from the body through the kidneys, but kidney function decreases with age. When kidney function decreases, drug levels can build up in the body, increasing the chance of side effects. Seniors are therefore more vulnerable to polypharmacy.
Common medicines that need to be used carefully in the elderly include diuretics, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen, and some blood pressure medicines including angiotensin converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs). Each of these medicines has effects on the kidneys; the effects can compound when these medicines are taken together. Close monitoring by doctors, pharmacists, nurse practitioners or physician assistants is important.
Keeping a list of all medications — including prescribed and over-the-counter drugs — that a senior is taking is important; seniors or their caregivers should share that list with each healthcare practitioner to prevent prescribing mistakes.
How often should seniors who use multiple medicines get their kidneys tested?
Dr. St. Peter: People aged 60 and above should have their kidney function tested every year or two, as kidney function declines with age. The test results of a blood test called serum creatinine are used to calculate a new value called the estimated glomerular filtration rate (eGFR). Doctors and pharmacists can determine how well the kidneys are working based on the eGFR, then decide which drugs to use and at what dosage.
Glossary:
Estimated Glomerular filtration rate (eGFR) is calculated based on a blood test called serum creatinine, which estimates how much liquid and waste is passing from the blood through the tiny filtering units in the kidney and out in the urine. eGFR varies depending on an individual’s age, race, gender and body size. According to the NKF, normal eGFR results range from 90-120 ml/min/1.73m2 and the levels decrease with age.
Urine albumin-to-creatinine ratio (ACR) measures the amount of albumin versus creatinine in urine. Albumin is a protein produced by the liver that retains water in the blood and should not be found in urine; persistent presence of albumin in the urine, therefore, indicates problems with the kidneys. The normal ACR is <30 mg/g (for everybody).
What drugs should be avoided if a senior has kidney issues?
Dr. St. Peter: There are many medications that should be used cautiously (with extra monitoring), or at lower doses in older patients with reduced kidney function. However, the risks or benefits of using a specific drug in an older person should be weighed by the patient and their healthcare team — doctors, pharmacists, nurse practitioners and physician assistants.
There are lists of potentially inappropriate medications (PIMs) that have been defined for older people, but there is no agreed-upon PIMs list for older people with reduced kidney function. This is why it is important for patients to keep an updated list of medications they are taking, and make sure that the list is shared with all of their healthcare professionals.
I encourage all seniors to have a primary physician and a pharmacist who are familiar with all of their medical conditions and medications. So every time a new medicine is considered, or whenever there is a medication change, a decision can be made with full knowledge of the complete picture.
How can someone with multiple chronic health conditions protect their kidney health?
Dr. Kramer: Avoid all NSAIDs like ibuprofen (Motrin®, Advil®) and naproxen (Alleve®), or use only sparingly. Keep blood pressure and diabetes under control. People living with diabetes or hypertension or who have a family history of kidney disease should test their kidney function and monitor urine for increased protein excretion with the albumin-to-creatinine ratio (ACR) every year.
Five Stages of Kidney Disease
The NKF developed a guide to identify the five stages of kidney disease. At Stage 1, although the kidneys are damaged, they are functioning at ≥90% of their capacity. The percentage of kidney function drops as kidney disease worsens. When the kidneys operate at less than 15% of their capacity, or at Stage 5 of chronic kidney disease, the patient is considered to have end-stage kidney failure. That is also when dialysis or a kidney transplant is needed to treat the symptoms.
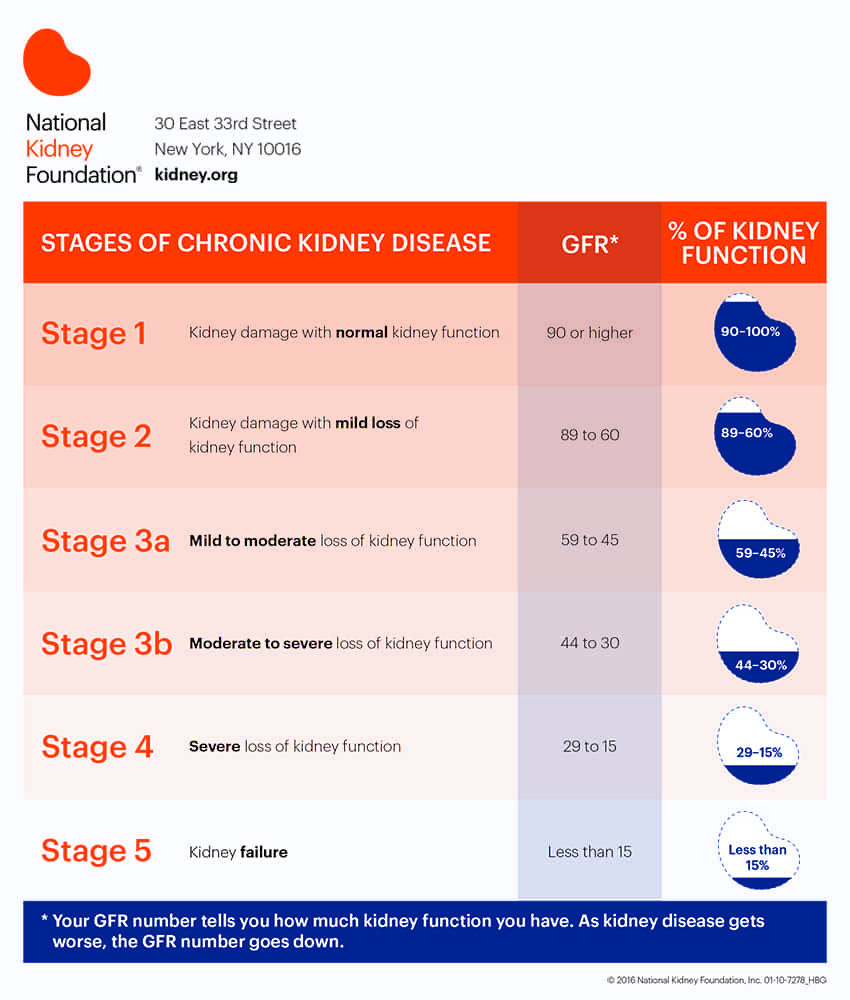
Photo courtesy of
National Kidney Foundation
.
Coping with end-stage renal disease (ESRD, or kidney failure) and ongoing treatment may be uneasy for many — support and assistance from family, friends or professional caregivers can be vital to the well-being of the patient.
How to care for someone on dialysis?
Dr. Kramer: Make sure the patient attends dialysis sessions as scheduled. Meet with a dialysis dietitian to get educated on diets for patients on dialysis, then help the patient follow dietary restrictions at home. Make sure the patient eats three meals per day including dialysis days.
Kidney Disease Management
Besides attending dialysis and recommended physician appointments as scheduled, patients on dialysis should also do the following to achieve satisfactory treatment results:
- Track the amount of liquid consumed in a day.
- Follow the prescribed diet.
- Ensure the doctor or nurse is checking the patient’s weight and blood pressure before and after each session.
- Confirm the patient’s care is evaluated on a regular basis.
Patients on dialysis may experience side effects such as fatigue, low blood pressure, anxiety and stress; emotional support from family, friends and/or caregivers will make a difference in their overall health.
Right at Home launched a disease management program in 2019, providing training to professional caregivers to support patients with renal disease. Services include transportation to and from the dialysis center, prescribed meal preparation3, medication reminders, monitoring changes in condition4, and implementing fall prevention and infection control strategies. A professional caregiver can also help record physician suggestions, monitor compliance with activities to occur in the home, and communicate changes or concerns to the supervisor and the client’s family.
1 Centers for Disease Control and Prevention. (2019). Chronic Kidney Disease in the United States, 2019. Retrieved from https://www.cdc.gov/kidneydisease/publications-resources/2019-national-facts.html
2 Charlesworth, C. J., Smit, E., Lee, D. S., Alramadhan, F., & Odden, M. C. (2015). Polypharmacy Among Adults Aged 65 Years and Older in the United States: 1988-2010. The journals of gerontology. Series A, Biological sciences and medical sciences, 70(8), 989–995. https://doi.org/10.1093/gerona/glv013
3 Caregivers can prepare or help prepare appropriate meals such as a low-salt diet, and fluid restriction per family instruction and monitor compliance.
4 Changes in condition can include reduced talking or alertness; newly agitated; confused or sleepy; shows any signs of pain; change in mobility; change in ability to stand or walk; observed or unobserved fall or slip; change in eating and drinking; change in chewing, swallowing or breathing; change in toileting; any discomfort, smell or change in frequency associated with urination, diarrhea or constipation; change in skin condition or increase in swelling; new skin rashes or wounds.



