Demystifying Dementia
“What is dementia?” The very first word that jumps into the brain of most people would be “Alzheimer’s” (or “memory problems”). But Teepa Snow wants us all to scrap that and remember: “dementia = brain failure.”
‘Dementia is a “neurocognitive degeneration,” a condition that needs chronic care,’ said Snow.
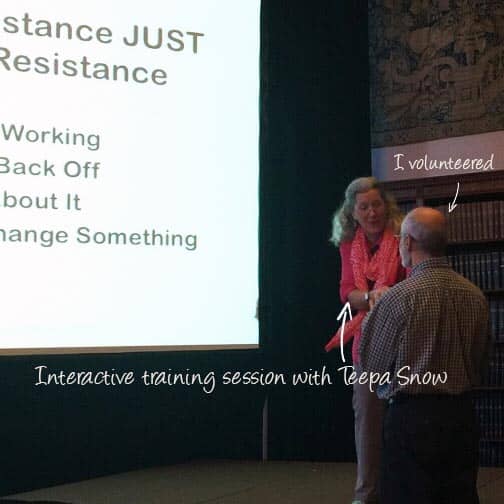
Teepa Snow is a dementia-care education specialist, who has extensive experience as a caregiver, occupational therapist, and trainer. This year, the New York Chapter of Aging Life Care Association invited Snow as the keynote speaker for its full day symposium at the New York Academy of Medicine.

Four of us from Right at Home – myself (representing the Lower Manhattan office), Leanne Feather (Lebanon, PA), Walter Ochoa (Brooklyn, New York), and Gregg Simons (Uptown, NYC) – attended the conference to demystify dementia.
Snow addressed in her speech that the decline in mental ability not only causes mysterious and challenging behaviors in dementia patients, but also affects the motor skills and cognition of sufferers. There were two main themes of the event:
- What is physically happening to the brain and how the sufferers sustain anxiety and or depression, and
- What we can do as caregivers to adapt to what skills and cognition they still have.
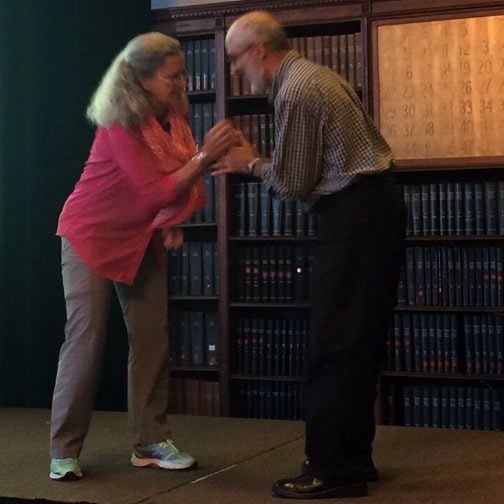
She invited volunteers to simulate how dementia patients behave on stage, and gave demonstrations of practical solutions / strategies for caregivers to adjust the behaviors.
1. Getting a dementia patient to think s/he is undressing herself/himself
- Approach the patient from the front (within her/his field of vision) and smile.
- Ask the patient if s/he is ready for a bath/shower using visual cues.
- Extend your hand in a friendly greeting and use the underhand. grasp (let the patient’s hand be on top). Keep your thumb and index finger free to unbutton/unzip.
- Cover the patient’s hand with yours and ask if s/he can help you with the buttons etc. You will be doing that with your two fingers but s/he may get the idea and finish undressing themselves.
2. Leading a patient from her/his dominant side
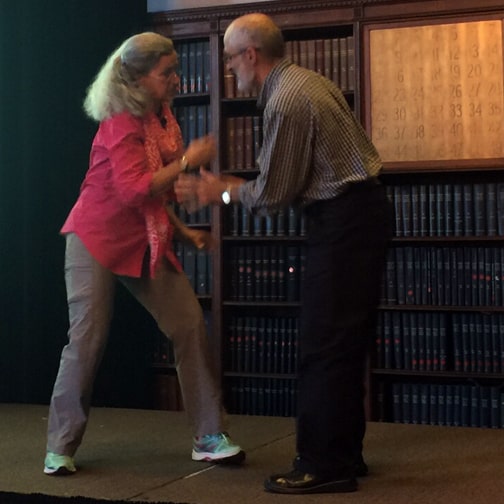
- Approach the patient from the front (within her/his field of vision). Greet the patient from outside of her/his personal space with a smile
- Extend a hand to shake, and convert that to an underhand grasp (let the patient’s hand be on top). Cover with your other hand.
- Switch your top hand to bottom, keeping the patient’s hand on top and apply gentle pressure to her/his palm.
- You can lead the patient by applying gentle pressure and pointing with your other hand. Since you are doing this from the patient’s dominant side, s/he will feel more comfortable.
3. Getting the patient to move even if s/he has some pain
Patients who are frail may stay still to avoid pain from movement, but that can render them frailer, even less mobile, and with a smaller range of motion. The pain usually subsides quickly once they are up and moving. You may get a patient to move by following the instructions below:
- Ask the patient for help, tell her/him you two are going to stand up together.
- Ask the patient to lean forward to center her/his weight over the knees.
- Acknowledge the patient’s pain when s/he is in a standing position, say “ow, ow, ow” repeatedly thereby making it unnecessary for the patient to say it.
As dementia patients lose self-awareness, they are not accurate in their perception. They struggle in their thoughts to make sense of daily activities and surroundings, sooner or later they become angry, frustrated, and even have anxiety or depression. Snow advised caregivers to focus on what the patient can do but not what the sufferers cannot do. ‘And build a team,’ continued Snow, ‘don’t try to be a “Lone Ranger.”’
Watch a keynote speech of Teepa Snow here: